Treating Mind and Body: Mental Health Care Expanding in Lesotho
Posted on Jul 24, 2018

It was a story no doctor wants to tell.
But at Botšabelo Hospital in Maseru, Lesotho, during a recent training on mental health care, a doctor related the story of a man who had successfully completed two grueling years of treatment for multidrug-resistant tuberculosis, or MDR-TB—only to succumb to a different, devastating illness, that far too often goes unseen.
That illness was mental, rather than physical, and likely involved severe depression. After beating MDR-TB by taking thousands of pills and enduring frequent, painful injections along with side effects including nausea, the patient was discharged by doctors at Botšabelo and returned to his home.
It was only there that, unemployed and lacking a support system of family and friends, he took his own life.
One-fifth of Lesotho’s 2.2 million people suffer from mental illness, according to a 2016 study led by Dr. Daniel Vigo of the Harvard School of Public Health, in work supported by PIH. That’s the highest rate of mental illness of any country in which Partners In Health works—but mental health is a need that crosses every border.
Lesotho also has one of the highest HIV rates in the world, affecting one in four people. Infectious diseases such as HIV and TB, and their treatments, are significantly affected by mental health, and mental illness.
“Mental health is the biggest total burden of disease, globally,” said Dr. Bepi Raviola, PIH’s director of mental health. “And diseases such as HIV and TB cannot be treated most effectively without considering mental health.”
That’s why PIH is ramping up its mental health programs in Lesotho and at PIH sites around the world, by training more providers to incorporate mental health into primary care and improving diagnosis and treatment for illnesses including depression, schizophrenia, epilepsy, and more.
Dr. Melino Ndayizigiye is clinical director for Bo-mphato Litsebeletsong tsa Bophelo, as PIH is known in Lesotho. He said the integration of care is vital in a country where the only mental health professionals are psychiatric nurses—usually just one or two for every 200,000 people, he added—and where many communities are in remote areas far from the nearest health facility.
“We cannot separate treatment of mind and body,” Ndayizigiye said.

The May mental health training in Lesotho, during which a doctor shared the tragic story of a patient’s suicide, was one part of an ongoing effort to bridge that gap, and followed a previous training there in August 2017. Dr. Stephanie Smith, associate director of mental health for PIH, led the first training session, while Dr. Todd Holzman, a Boston-based psychiatrist, led the second. Doctors and nurses participated at Botšabelo Hospital in Maseru, Lesotho’s capital, and at a regional hospital in the district of Mohale’s Hoek, south of Maseru.
The trainings’ goals included raising clinicians’ awareness of mental illness among patients and improving their diagnostic skills. They learned to screen patients and monitor progress, identify symptoms of depression during pregnancy, and recognize common mental health concerns among different age groups.
Holzman said that, ultimately, much of the work is rooted in listening to patients, asking them how they’re feeling, and understanding the social and familial scenarios that can affect their health. Some people might show signs of depression that actually stem from medical conditions.
“Be sure you eliminate that possibility before you initiate treatment,” Holzman said. “A depressed mood can be caused by a number of medical conditions, such as hypothyroidism, early pancreatic cancer, or Parkinson’s disease—to name just a few.”
Dr. Lawrence Oyewusi, MDR-TB program manager at Botšabelo, said his staff appreciated the sessions.
“It was an intensive training but interactive, where people were able to discuss, share their experiences and ask questions,” Oyewusi said.
Staff at Botšabelo said some MDR-TB patients can exhibit severe depression or even psychotic behavior as a side effect of the powerful drugs, and depression also can affect patients’ families. Several doctors emphasized the need to strengthen mental health training and extend care not only to patients, but also to family members and caregivers.
“Given that patients suffering with MDR-TB and HIV/AIDS are desperate, often depressed, and already taking more than a dozen medications daily, it is essential that we raise the capacity of health care providers at all levels to screen for psychiatric disorders, especially depression,” Ndayizigiye said.



Oyewusi’s team has a plan in place to screen all patients for mental health. He said that, anecdotally, depression is the most prevalent mental health disorder at Botšabelo, where patients struggle with two years of treatment coupled with high co-infection rates for HIV, diabetes, renal failure and more.
He said the screening process will provide stronger data for rates of depression and other mental health disorders.
More successful treatments and broader awareness about mental illnesses also could go a long way toward changing societal perceptions.
Smith told Botšabelo staff that stigma and discrimination against people with mental illness can create significant barriers to treatment.
“Stigma can lead to neglect, physical abuse, denial of access to help and a violation of an individual’s human right to quality health care,” she said. “It’s important that we address stigma on all levels. Getting people the treatment they need, including successful reintegration into the community, demonstrates that mental disorders are treatable. That is one of the most important stigma-busting activities that we can support.”
PIH is spreading that message on an increasingly large scale.
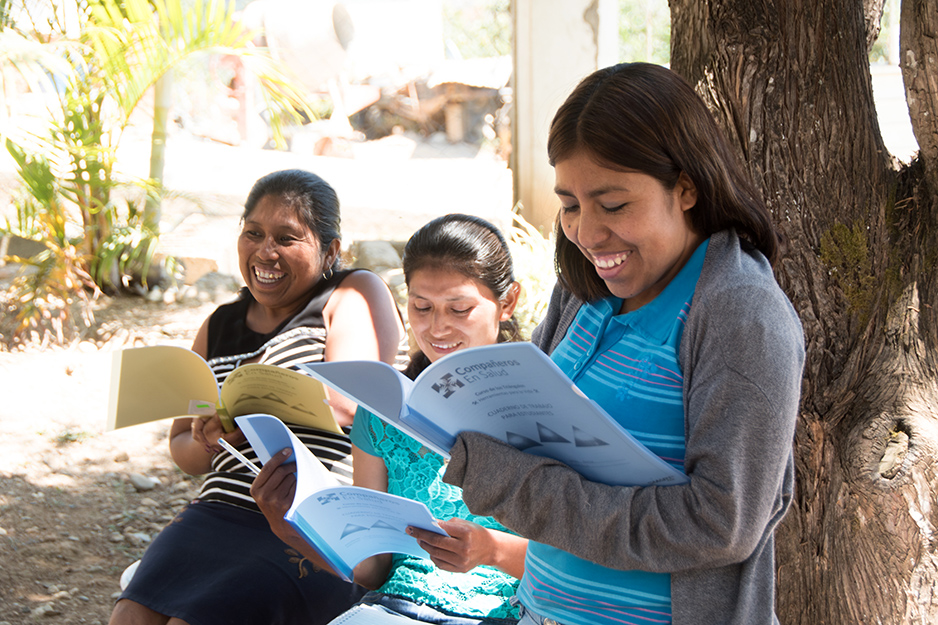
PIH’s largest mental health programs are in Haiti and Rwanda, which each have more than 3,000 patients. Socios En Salud, as PIH is known in Peru, has expanded its program significantly in recent years and is piloting a safe house program, for example, that the government has adopted and is scaling nationally, to 350 locations. Compañeros En Salud, as PIH is known in Mexico, has incorporated mental health care since 2011, when it began operating in the mountainous region of Chiapas, and also has expanded its program in recent years.

PIH also is supporting growing mental health programs in Liberia, Sierra Leone, and Malawi.
Often, that growth is from the ground up. Raviola said in most countries where PIH is supporting the development of mental health care, the field is not taught in medical or nursing schools. Nearly all patients have few, if any, options for treatment.
“In the countries where we work, we’re often starting from scratch, but, in collaboration with local Ministry of Health teams, we’re making rapid progress in piloting effective, community-based mental health care delivery systems,” Raviola said.
Additionally, in collaboration with a new Harvard University initiative called GlobalMentalHealth@Harvard, PIH is bringing together front-line organizations who are proving that mental health treatment can be delivered in low-resource settings. In June, Raviola and Professor Vikram Patel of Harvard Medical School— supported by the Harvard Medical School Center for Global Health Delivery-Dubai—led a meeting focused on increasing the role of community health workers in mental health care. Representatives from all PIH sites participated, along with leading researchers and members of nongovernmental organizations in India, Bangladesh and Pakistan.
Oyewusi said that in Lesotho, improving the availability and quality of mental health care comes down to a universally common need: more resources. Specifically, he said, more “staff, space, supplies and systems.” That PIH mantra applies to health care delivery across the board, whether it’s for TB, HIV, maternal health or mental health.
And the same motivation for that care—that health is a human right—applies to mental health as much as any other condition.
“People get better,” Raviola said, “and it has a truly remarkable and transformative effect on attitudes and beliefs.”

