We Demand Justice in Health Care
Everyone should have access to quality health care. But for millions around the world, that’s not the reality.
FOLLOWING PAUL’S VISION
Dr. Paul Farmer (1959-2022) co-founded Partners In Health based on the belief that everyone deserves quality health care. Paul cared for the sick, trained generations of clinicians, and transformed health care policies–saving millions of lives and inspiring a movement toward global health equity. We carry forward his legacy and vision.
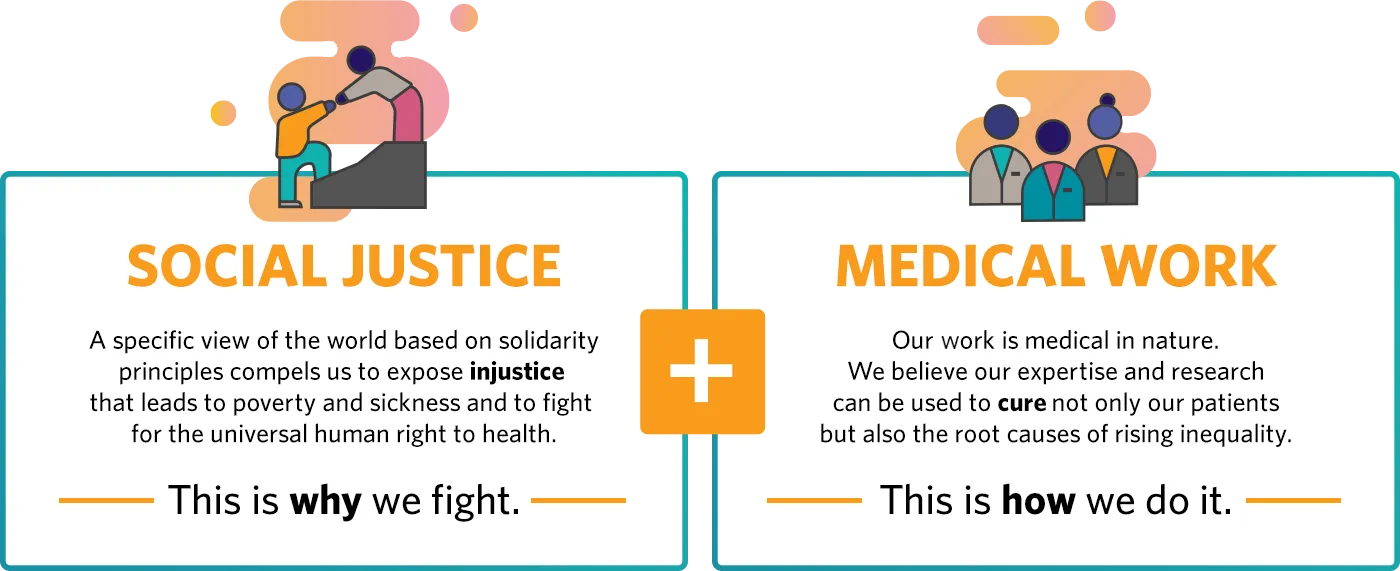
WHAT DRIVES US
We are a global health and social justice organization that responds to the moral imperative to provide high-quality health care globally to those who need it most.
We strive to ease suffering by placing patients at the center of all care, meeting not only their physical, but also their mental, emotional, and daily needs so that they can recover from illness and maintain good health.
We bring the benefits of modern medicine to those who have suffered from the overt and subtle injustices of the world, in the past and in the present.
We refuse to accept that any life is worth less than another.
YOUR IMPACT ON GLOBAL HEALTH INEQUALITY
With your support, Partners In Health delivered health care to the world's most impoverished places, partnering with local governments to bring about global change. Last year, we provided:
Over 2.1 million home visits by community health workers.
821,000 COVID-19 screenings from borders to clinics to homes.

2.1 million women’s health checkups around the world.
2.8 million outpatient visits in supported clinics.

