Mental Health
The World Health Organization estimates that one in eight people in the world live with a mental disorder. However, on average, countries dedicate less than 2% of their health care budgets to mental health, and around half the world’s population lives in countries where there is just one psychiatrist to serve 200 000 or more people. And the availability of affordable essential psychotropic medicines is limited, especially in low-income countries. Most people with diagnosed mental health conditions go completely untreated. In all countries, gaps in service coverage are compounded by variability in quality of care.
Investing in mental health for all advances public health and enables social and economic development. It can greatly reduce suffering and improve the health, quality of life, functioning and life expectancy of people with mental health conditions. Evidence shows that there is a core set of cost–effective interventions for priority conditions that are feasible, affordable and appropriate.
Transforming mental health means strengthening community-based care for all in need. This means shifting the locus of care for severe mental health conditions away from psychiatric hospitals towards community-based mental health services. At the same time, care for common conditions such as depression and anxiety must be scaled up. Both strategies are critical to improve coverage and quality for mental health care. People-centered, recovery-oriented and human rights-based care is essential.
PIH’s Response
The OnePIH Mental Health Program seeks to improve the lives of the patients and communities we serve by expanding the continuum of mental health and psychosocial support services available across all PIH care delivery sites around the globe. The OnePIH Mental Health Team strengthens primary care, and hospital-linked mental health systems to provide collaborative, comprehensive, community-based mental health services for common, complex, and co-morbid mental health conditions in settings where few to no services are otherwise available.
Over the past decade, PIH has created a substantial, measurable, innovative global mental healthcare delivery model that has the potential to be scaled up nationally in partnership with local communities, governments, and Ministries of Health. The team’s Mental Health Service Planning Matrix guides improvements in mental health service availability, access, and quality for hundreds of thousands of people. Moreover, challenges in global mental health delivery and opportunities for capacity building are shared across global settings through PIH’s Mental Health Learning Collaborative.

Mental Health Service Planning Matrix
The PIH Cross-Site Mental Health Matrix to Achieve Universal Health Coverage is a blueprint for global mental health care delivery. It is a planning tool to expand service delivery and model effective implementation of mental health services at national referral hospitals, district hospitals, health centers, and community levels.
Our Mental Health Programs
All 11 PIH sites have established formal mental health teams and programs. The teams articulate functional models of mental health care services focused around 4 theory of change themes:
- Asserting quality of Mental Healthcare Across settings
- Training and Education for mental health professionals through partnerships with high quality clinical, education, and research institutions
- Influencing with Evidence through targeted research, impact dissemination, and quality imjprovement methodology local systems
- Scaling up the PIH mental health care delivery model with government partners
In partnership with the Program in Global Mental Health and Social Change and the Dr. Mario Pagenel Fellowship in Global Mental Health Delivery at Harvard Medical School, PIH is building platforms for the delivery of safe, effective, evidence-based, and culturally sound mental health services everywhere it works Here are just a few examples of how the PIH mental health teams bring mental health care, awareness, and education to communities around the world.
Rwanda
Inshuti Mu Buzima/PIH Rwanda supports community-based mental health care in rural public primary care systems in Rwanda’s Kirehe, Kayonza, and Burrera Districts using task-sharing models for psychotherapy, psychosocial rehabilitation, mentorship, training, and supervision. They partner with the University of Global Health Equity to train the next generation of practitioners on how to provide holistic, human-centered mental health care.
Haiti
In collaboration with the Ministry of Health, Zanmi Lasante/PIH Haiti psychologists, social workers, nurses, physicians, and community health workers employ a task-sharing model to integrate mental health services into primary care for a catchment area of over 1.5 million people.
Peru
Socios en Salud/PIH Peru psychologists integrate mental health care into maternal health, tuberculosis, early childhood development, and chronic care programs using innovative technology and support the Ministry of Health to scale interventions at the national level.
Mexico
Companeros En Salud community mental health workers deliver psychotherapeutic interventions for depression and anxiety, conduct psychoeducation groups, and work with adolescents in the community. Community members promote restorative justice & gender equity through locally established women’s circles and men’s support groups.
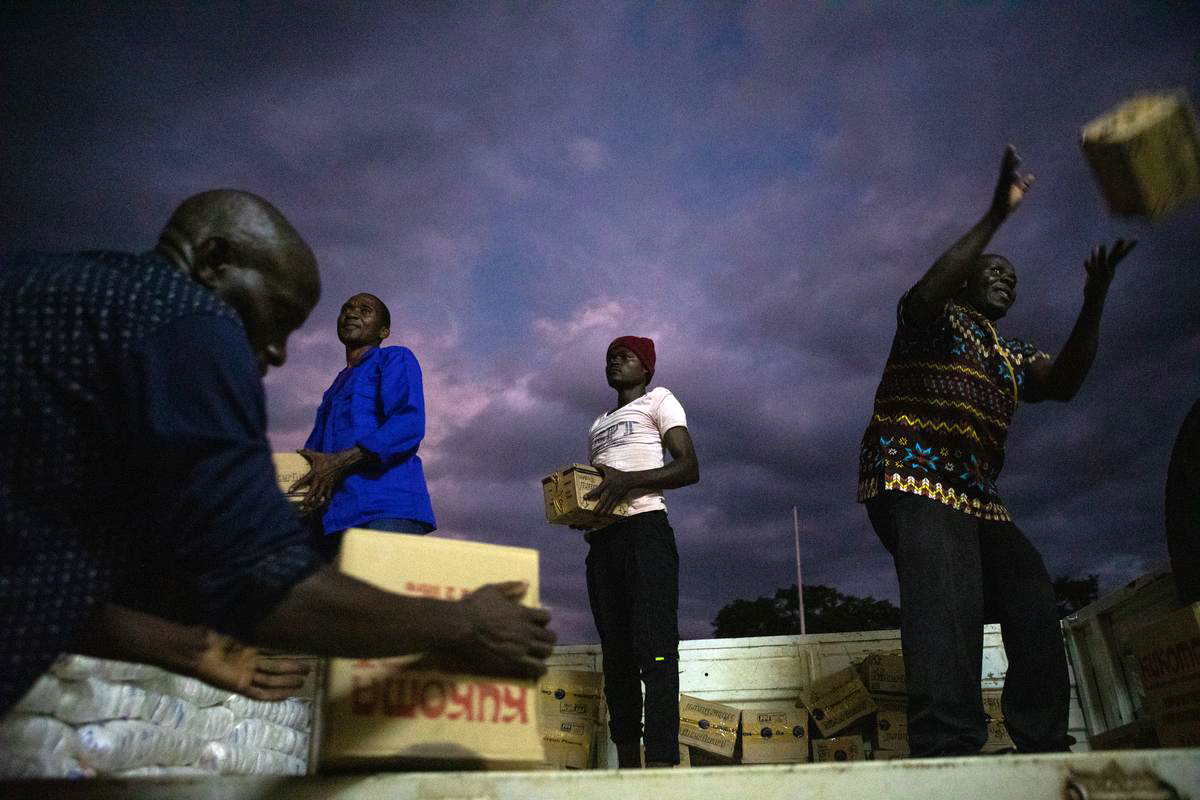
Liberia
PIH Liberia’s close partnerships with community members, traditional healers, lay providers, and facility-level providers strengthen the quality and reach of mental health services. Peers and caregivers lead psychosocial rehabilitation groups, and PIH works with the Ministry of Health to revise national mental health policy.
Sierra Leone
PIH Sierra Leone integrates psychiatric and psychological care into the community, primary care, and district levels. It also supported the transformation of the oldest asylum in subsaharan Africa’s into the nation’s first Psychiatric Teaching Hospital, which provides care to youth and adults, and hosts the country’s first psychiatric residency program to train the next generation of Sierra Leonean psychiatrists.
Malawi
Abwenzi Pa Za Umoyo integrates mental health care into its care pathways for patients with chronic conditions. Psychologists and lay counselors provide group psychotherapy for maternal depression.
Lesotho
PIH Lesotho counselors, nurses, and psychologists deliver psychosocial interventions and integrated care for depression, MDR-TB, and crisis response. The team helps lead the Technical Working Group responsible for the drafting of Lesotho’s first national mental health policy and strategic plan.
Kazakhstan
Psychologists and social workers integrate depression care for patients with MDR-TB and implement substance use prevention activities for university students.
Navajo Nation
The Community Outreach and Patient Empowerment Program (COPE) in the Navajo Nation collaborates with local partners to increase access to mental health resources for community members and front-line workers.
Russia
The PIH-supported NGO in the Vladimir region provides psychosocial support and counseling to tuberculosis (TB) patients and other persons in need. The team uses online services to screen and enroll patients from other regions.
United States
The Cross-Site Mental Health team is partnering with PIH-US and organizations throughout the country to adapt lessons learned from PIH’s care delivery sites to the US context. The team provides mental health training, technical assistance, and implementation support to PIH-US regional teams and community-based organizations around the country.
Our Impact
105 PIH-supported facilities deliver mental health care across all 11 PIH sites.
More than 70,990 patients received treatment for mental health conditions between 2016-2023.
PIH's impact through evidence-based interventions has increased eight-fold from 2018 to 2023.
Mental Health Programs
We are helping thousands of patients around the world through innovative programs — proving that high-quality mental health care can and should be available to all people, no matter where they live.
Featured Mental Health Videos