One Mother's Fear in Lesotho: Will My Newborn Also Live With HIV?
Posted on May 8, 2018

Thabo Lerata* was born at 1 p.m. on Jan. 1, 2018, the first baby of the New Year to be delivered at Holy Cross Health Center in the highland district of Mohale’s Hoek, Lesotho.
His 36-year-old mother, Mathabo Lerata,* made quite a trip to bring him into the world.
Lerata left their home around 9 a.m. that day—while in the early stages of labor—to begin walking to Holy Cross. The trip would require crossing a broad field atop a plateau, then descending a switchbacking dirt road to the closest paved road, at the bottom of a steep slope. She carried a few belongings as the hot day began.
January is the heart of summer in the Southern Hemisphere, and the sun can beat down heavily on the high-altitude ridges of Mohale’s Hoek, in Lesotho’s southwest. South Africa entirely surrounds Lesotho, a small, agricultural nation that proudly calls itself the Mountain Kingdom.
Partners In Health (PIH), known in Lesotho as Bo-mphato Litsebeletsong Tsa Bophelo, has worked in the country for more than 12 years. That work significantly expanded in 2014, when PIH began supporting Lesotho’s national health reform, as the primary technical advisor to the Ministry of Health. The reform’s goals include reducing child mortality and mother-to-child transmission of HIV, improving maternal health, and combating HIV and TB, of which Lesotho has some of the world’s highest prevalence rates. PIH and the ministry are piloting the reform in four districts, including Mohale’s Hoek, but the goal is to expand nationwide and ensure that all of Lesotho’s 2.2 million people have access to health care, in the most remote locations.

The Leratas’ one-story home fits that description.
It would take Lerata more than an hour to reach the PIH-supported Holy Cross on New Year’s Day. Stepping out her front door, she had views all around of rugged mountains that sometimes resembled the American Southwest. She first crossed the top of the plateau—a wide field strewn with large rocks, patches of dirt, and thin, faded tracks. Lerata later said it can get very windy up there, and very cold in the winter. On clear days, she can see across the nearby border into South Africa. On the other side of the plateau is the village of Ha Mohlekana, a small cluster of homes and buildings near the dirt road that leads down the slope.
Lerata makes the walk all the time, as do her 15-year-old daughter and 7-year-old son, and said the trip from her door to pavement takes about 30 minutes. That seems optimistic at first glance, but she’s lived there for more than 13 years and says it confidently—30 minutes.
From the paved road, it’s usually 30 more minutes by foot to Holy Cross.
Unless, of course, you’re pregnant. Or in labor.
Lerata said her contractions with Thabo started Dec. 31, but she initially didn’t realize they were contractions, because they felt different than they had with her first two children.
Her first two children were born at the district hospital in Mohale’s Hoek, farther away from the family’s home than Holy Cross.
The proximity of the health center—relative proximity, at least—was a blessing with her third child.
Lerata's village health worker, Malerato Tsoelesa, had visited her at least twice a week since before her pregnancy with Thabo. Tsoelesa regularly checked on the entire family, to accompany Lerata and her children to the PIH-supported Holy Cross for free doctor visits, and then to guide Lerata's prenatal care. In all, Tsoelesa works with seven families around the village. All of them have children.

But Tsoelesa wasn’t able to be at Lerata’s home that morning, because things happened so quickly. Lerata’s husband was away in South Africa, working in mines.
The resulting situation was vastly different from labor and childbirth in the U.S.—and most other countries around the world, for that matter. Walking such a distance and in such rugged conditions while in labor, or even late in pregnancy, would be unthinkable.
But not in Mohale’s Hoek.
Lerata told the story offhandedly six weeks later, sitting in her living room and holding Thabo on her lap. She didn’t say whether she had been alone on the morning he was born, or whether she had taken a taxi from the paved road or just continued walking to the health center.
Those details didn’t seem to matter all that much.
Lerata acknowledged that people often exclaim when she tells the story of that day, but said she shrugs it off, herself, saying the walk wasn’t too bad because her labor started gradually.
Besides, as she told the story on the morning of Feb. 13, she had something else on her mind. Thabo was due for his six-week checkup at Holy Cross, which would include a PCR test (the acronym stands for polymerase chain reaction). The test would be held the next day, and Lerata would be able to see the results within about an hour, during the same visit.
The test would be the first indicator of whether Thabo had HIV, like both of his parents.
Lerata said her husband learned he was HIV-positive in 2008, and has been on antiretroviral therapy (ART) since about that time. She was diagnosed a year later, and also started ART promptly.
Both of their older children are HIV-negative. Those results and both parents’ commitment to ART meant Thabo’s odds were good, too. But there was still a risk.
Dr. Afom Andom, PIH’s lead technical advisor for Lesotho’s national health reform, said that without ART, the risk of pregnant women with HIV passing the virus to their children can reach 40 percent. Transmission can occur in utero, during childbirth and while breastfeeding.
Lesotho's Ministry of Health and PIH are taking significant steps to reduce that rate. Andom said a scaled-up HIV program, begun in 2016, has made Lesotho the first country in sub-Saharan Africa to implement widespread screening practices known as “test and treat.” The increased screening and a corresponding emphasis on long-term, sustained ART have combined to reduce mother-to-child transmission to less than 6 percent, across 72 health centers in the reform’s four pilot districts. The goal is to ultimately achieve a rate of less than 2 percent.
Lerata consistently uses Holy Cross for her ART and services for her children—all three of them have received immunizations, checkups and more at the health center.
On the morning of Thabo’s six-week checkup and PCR test, Lerata brought him to Holy Cross in a taxi. She said the trip cost 6 South African rand (US$0.50). The rand is commonly used in Lesotho, along with the national currency, the loti.
The mood inside Holy Cross that morning was festive. It was Valentine’s Day and several of the nurses were wearing red, some because of the holiday and others just because.
Rain began falling against a window as Lerata fed Thabo in a clinic room around 10 a.m. He was fussy and hungry, which his mother described as common. He had been crying, eating and moving around more than his two older siblings had when they were infants.
As registered nurse midwife Mamakama Mofolo began the checkup, Thabo soon began crying again.

“Phephi, phephi (Sorry, sorry),” Mofolo said softly, as she checked Thabo’s head circumference, bone development, body length and more, moving from head to toe and repeating the Sesotho apology, pronounced like “peppy.”
As Thabo fussed, another baby could be heard crying in the hallway. Holy Cross serves more than 11,550 people, from villages throughout the region, and was busy that Wednesday morning.
After the checkup, Lerata fed Thabo again, quickly calming him down. Then it was time for his PCR test.
Four counselors were waiting in a small room across the hall. Marelebohile Motlomelo, Makanelolo Mahlatsi, Nthabeleng Ichasake and Matseko Mokhamo gave Lerata pre-test counseling, advising her on the procedure and what the results would mean.
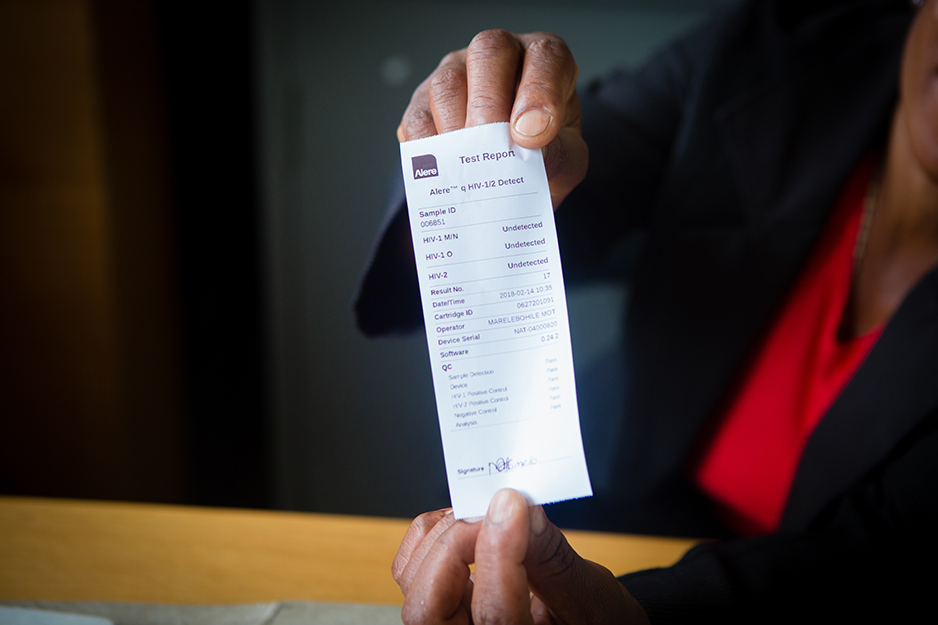
Motlomelo then leaned forward and made small pricks in one of Thabo’s big toes, drawing a few drops of blood. She used a container that resembled a floppy disk to absorb the sample, then placed the container in the health center’s PCR machine.
It’s rare for health centers in Lesotho to have such a machine—most often, samples are sent to district or national labs for analysis. The machine at Holy Cross is supported by multiple aid partners, in response to the high number of infants exposed to HIV in Mohale’s Hoek.
Processing Thabo’s results would take about an hour.


In the meantime, Lerata brought her son into a larger room at the health center, for immunizations. Several other mothers held infants in the room, sitting in rows of chairs while waiting for shots.
When it was Thabo’s turn, Nurse Assistant Mookho Matekane kneeled by their chair and gave him vaccines against polio and pneumococcal conjugate, along with a pentavalent, which combines five vaccines into one shot.
Thabo didn’t like the shots, understandably, and began to cry again. It was about 10:50 a.m., less than an hour after he and his mother had arrived at Holy Cross. The healthy, active 6-week-old had had a tough morning.
And it undoubtedly was just as hard for Lerata, as she waited at the health center for PCR results. Infants at risk for HIV also are tested at 14 weeks and at nine months, and then given a definitive test at 18 months, so Thabo’s results that day would be preliminary. But Dr. Andom said the six-week results are a strong early indicator of an infant's status. Changes of that status in later tests are rare.
Soon enough, Thabo’s results were ready.
Lerata returned to the counseling room, and sat in a chair next to a desk. Motlomelo read the results out loud.
HIV-negative, just like his brother and sister.
Lerata’s eyes watered, and a smile broke across her face. She laughed and took a deep breath, as the results were written in a register and in Thabo’s bukana, a small book kept by the family that contains a child’s birth information, medicines and health history.

All of the counselors smiled as everyone leaned back in their chairs, a morning’s worth of tension palpably erased.
“Kea leboha (Thank you),” Lerata said in Sesotho. “Kea leboha.”
The rest of their visit passed quickly. Lerata walked outside to the adjacent, one-room HIV facility, where she received a refill of her ART. A large filing cabinet had drawers labeled for active ART patients, pre-ART, and more.
Next door, pharmacist Malefetsane Letsosa filled the prescription.
Outside, Mary Lesesa, the primary health care coordinator for Mohale’s Hoek, translated more of what Lerata had said in Sesotho after the PCR results were read.
“She was a bit frightened,” Lesesa said. “But when the results came out, she was very happy."
That emotion was evident as Lerata prepared to leave the health center. She swept Thabo onto her back, snuggled into a baby carrier, and wrapped him securely there with a large, brown-and-peach blanket.
Then Lerata, her 7-year-old son—who had come along that morning—another mother, and Tsoelesa, Lerata’s village health worker, left Holy Cross and proceeded up the road, talking and laughing as they began another long walk home.
* Names have been changed.


