In Peru, Partners In Health Provides Key Evidence for Global Mental Health Manual
After being validated by Partners In Health in Peru, a mental health training model launched by the WHO, UNICEF, and George Washington University is now a global benchmark.
Posted on Jan 13, 2026

Editor’s note: This article was originally published in Spanish on Socios En Salud’s website.
For decades, mental health has been a blind spot in public health systems. In low- and middle-income countries, such as Peru, only 3 out of every 100 people with depression receive treatment, largely because there are not enough specialized professionals, according to the World Health Organization (WHO).
To start to address this challenge, the WHO and UNICEF, in academic partnership with George Washington University, launched the Foundational Helping Skills Training Manual (FHS) in July 2025. The manual aims to equip doctors, nurses, social workers, and other community stakeholders with simple but essential tools to provide safe and effective support when interacting with adult patients.
FHS is part of an initiative from the same organizations called Ensuring Quality in Psychological Support, more commonly known as EQUIP. EQUIP proposes a new competency-based approach to mental health care: teaching specific skills—such as active listening, empathy, and conveying hope—and evaluating them in practice, not just through theoretical exams. It’s a flexible, widely applicable, and evidence-based method.
“EQUIP is many things, but above all, it's a response to the lack of standards that guarantee safe and high-quality mental health care. It's a paradigm shift,” said Dr. Gloria Pedersen, director of mental health and psychosocial support at Partners In Health (PIH), a researcher at Harvard Medical School, and one of the project leaders.
Socios En Salud (SES), as PIH is known in Peru, was a key part of this change in approach. SES’s work helped test EQUIP’s methodology before and during the pandemic, proving its effectiveness even during the most critical moments, with remarkable results. What began as a local initiative is now part of a global manual poised to transform the way the world approaches mental health.
What is EQUIP?
In the early 2000s, a simple yet powerful idea gained traction in mental health: sharing clinical tasks with non-specialized personnel, like community health workers. Promoted by the WHO and various universities, this approach spread to countries with fewer resources, bringing support to communities that often experience a shortage of trained professionals.
The challenge, however, was how to ensure that those providing psychosocial support—whether mental health specialists or not—offered safe and high-quality services. There was no clear way to assess this standard of care.
With this need in mind, EQUIP was born: a digital platform that seeks to improve mental health care and psychosocial support. Through simulations, direct observation, and feedback, EQUIP teaches and evaluates key skills, prioritizing how they are applied in practice, not just in theory. It's not simply a checklist, but a training philosophy.
"We designed a tool that allows us to measure skills, integrate them into training and supervision, and promote a competency-based approach that goes beyond simple knowledge tests," Pedersen said.
EQUIP fills a crucial gap by offering a standard valid for psychiatrists and psychologists, as well as community workers around the world.
“The main challenge, as is often the case, was funding, in which USAID initially played a key role,” says Dr. Pedersen. “Another challenge was adapting the tools to multiple cultural and linguistic contexts, as we worked with more than seven countries on rigorous research to ensure they were valid and useful in different settings.”
Fortunately, SES and PIH were able to use existing resources and decades of experience to support this part of the project.
The Role of PIH in EQUIP’s Success
Before the pandemic, talking about mental health in Peru was difficult.
“There was a very strong stigma," said Carmen Contreras, head of the Mental Health Program at SES. In rural areas, almost half of women and more than a third of men feared being judged if they sought psychological help, which limited access to services.
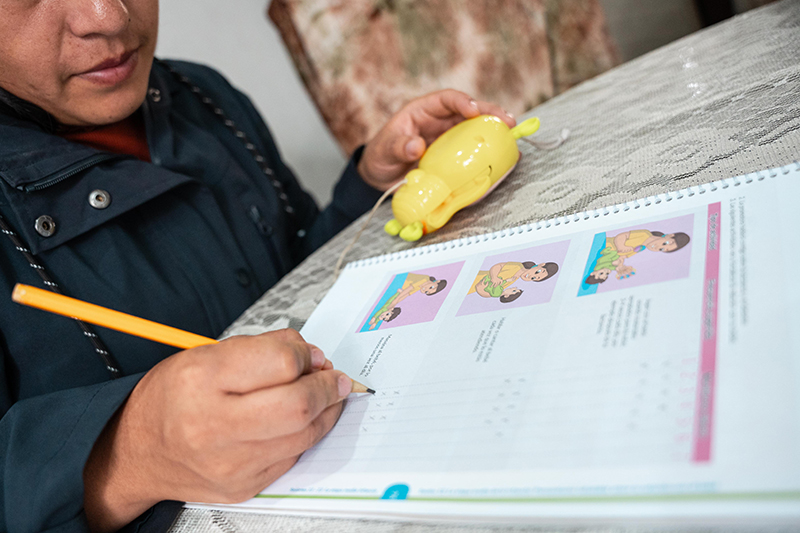
With this context, it was surprising when Peru was chosen as one of the countries in South America to carry out EQUIP. The implementation was carried out through an existing project called Thinking Healthy (PENSA), led by SES's mental health program and aimed at women with perinatal depression in northern Lima. It was the first time that a global tool of this type had been tested in Peruvian communities.
“In addition to providing training, EQUIP allowed us to evaluate the entire intervention process, which was still under development,” Contreras said. “For me, it was an opportunity to position SES as a leader in the skills that every mental health professional should have, beyond traditional technical or academic training.”

From Dr. Pedersen's perspective, SES was crucial to EQUIP’s overall success.
“They adapted the tools to the Peruvian and Spanish-speaking contexts, and even co-developed specific instruments for the PENSA project,” she said. This flexibility allowed the practical integration of learning into community health services.
This effort became especially important with the arrival of the pandemic. Faced with restrictions and lockdowns, SES’s mental health program began utilizing innovations like chatbots and other remote tools to support the community through both specialized and non-specialized mental health professionals, including community health workers. These digital solutions ensured the continuity of psychosocial support at a time when the need was more urgent than ever.
The reach was remarkable. In addition to validating the methodology, SES contributed to the development of the FHS, an essential part of EQUIP's resources. With this collaboration, the training also reached professionals without prior training in mental health—nurses, midwives, and students—expanding the project's impact.
"The impact was so significant that many professionals said it was the first time they had learned how to address suicide in a practical way," Pedersen said.
From Practice to Systemic Change
The FHS manual, which incorporates the EQUIP model, opened up an unprecedented opportunity for SES. After its initial success with PENSA, the team is now preparing to implement the tool in other local interventions.
"As always, we want to start in Carabayllo [a district north of Lima]," Contreras said. "The idea is to demonstrate results and then present them to the Ministry of Health."
This transition from the local to the national level is precisely what excites Dr. Pedersen. For her, EQUIP is changing the way mental health professionals are trained on the front lines.
"The most impactful thing was seeing nurses and midwives applying what they had learned weeks later, especially during suicide risk screening, on their own initiative," she said.
EQUIP’s success lies in its approach. It's no longer about imparting theoretical knowledge that often remains purely academic but about developing observable and practical skills. Through simulations, feedback, and role-playing, professionals not only learn what to do, but also how it feels from the patient's perspective. This level of empathy changes the way care is provided.

The next challenge is to systematically demonstrate the impact of EQUIP—both locally and on a global scale.
“There is already evidence that EQUIP’s approach reduces harmful behaviors and promotes helpful practices among providers,” Pedersen said. “What's missing is direct data on the patients themselves. We want to compare, for example, two groups of nurses, one trained with these competencies and the other using the traditional method, and analyze the clinical outcomes.”
Although the pandemic slowed down some of the studies, many of the results have been promising. In India, patients treated by professionals trained with simulations had better outcomes. In Nepal, a cost analysis showed that this approach is not only more effective but also does not increase training costs.
"The evidence suggests that competency-based training is more useful and sustainable," Pedersen said. "Now, we are working to integrate these skills into undergraduate and graduate programs.”
This is the type of systemic change that Partners In Health and Socios En Salud strive for: improving care at every level for people around the world, especially those most vulnerable.
Support Our Work
We believe quality health care is a universal human right. Around the world, we fight injustice by providing care to those who need it most.

