Four Pillars of PIH’s Work in Malawi
Community and mental health, social support, HIV, sexual and gender-based violence among key program
Posted on Mar 28, 2022

Malawi has been in the news for powerful cyclones and other extreme weather that has battered homes, clinics, communities and farmland. But the country is also recognized for other reasons, including innovative approaches to delivering comprehensive health care in remote communities.
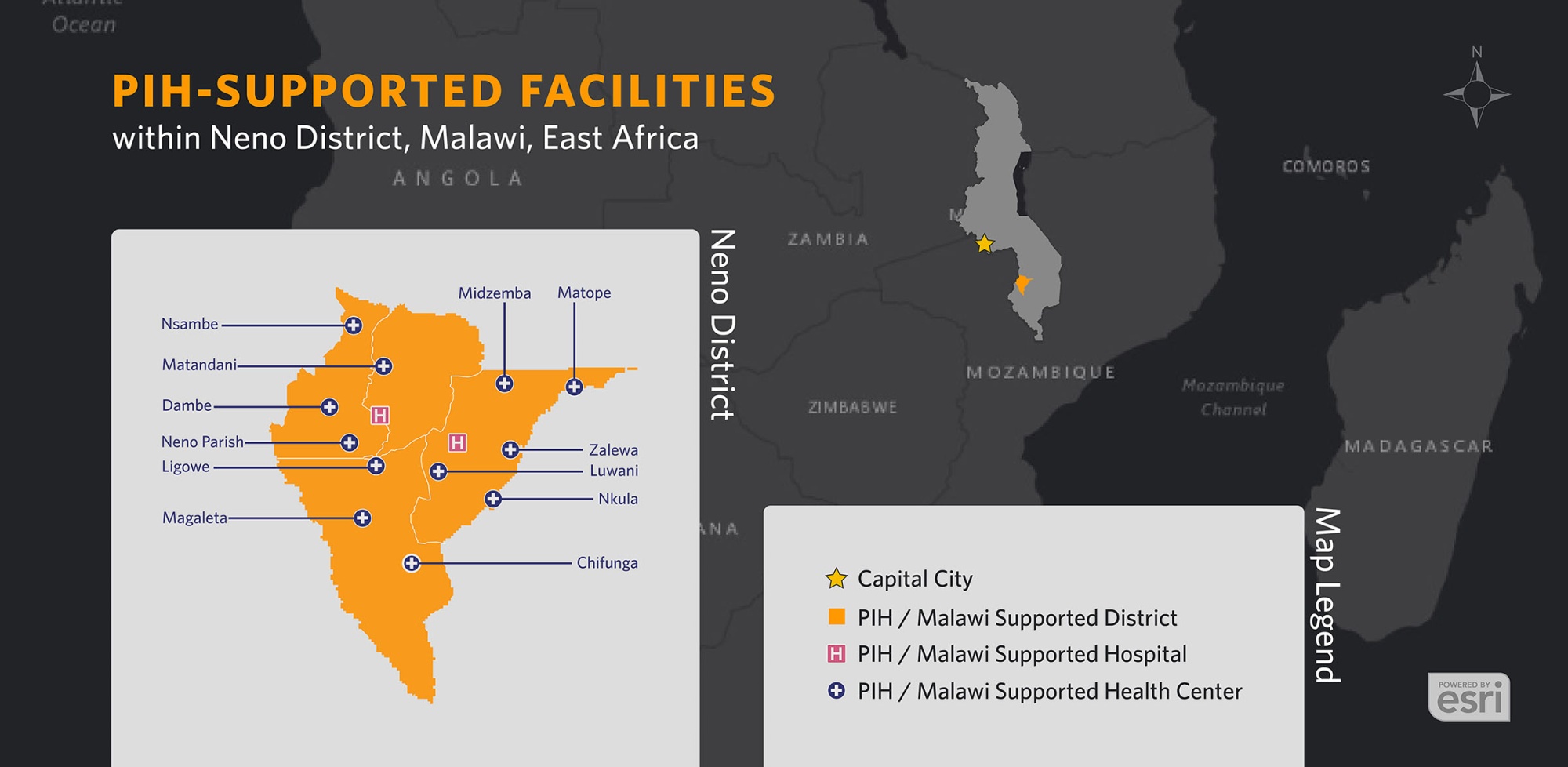
Abwenzi Pa Za Umoyo, (APZU), as Partners In Health is known in Malawi, has worked in the landlocked nation in southeastern Africa since 2007. Focusing efforts in Neno District, a rural, remote area of approximately 165,000 residents, where tarmac roads remain a work in progress, and just over 3% of households have electricity, the APZU team has developed effective models of integrated health care to deliver top quality treatment and critical social services to patients. Together, the efforts have led to measurable improvements for people afflicted with HIV/AIDS, mental illness, chronic conditions, and more.
Barriers Abound
Life in Malawi can be harsh: it’s one of the most impoverished countries in the world, with a daunting HIV epidemic, a significant non-communicable disease burden, and high rates of infant and maternal mortality, as well as sexual and gender-based violence. Making matters worse, access to decentralized, high-quality care is scarce or unaffordable for most people. Even those who can pay for treatment are often unable to reach clinics, especially over mountainous terrain and rugged roads in remote areas.
In response to these challenges, APZU is building and supporting a model of free, accessible, one-stop-shop health care in Neno District through two hospitals, 12 health centers, and a network of 1,228 community health workers (CHWs) offering treatment for everything from HIV and malnutrition, to mental health support and diseases such as hypertension, diabetes, and sickle cell anemia.
Below are four of APZU’s key programs:
Social Support
A pillar of APZU is its Program on Social and Economic Rights, (POSER), which empowers community members to live with dignity, security, and independence. POSER delivers cash assistance to help patients address costs related to health care, ensuring that Neno’s most vulnerable have access to medical care and the basic necessities to stay healthy, such as housing, employment, education and transportation.
CHWs and clinicians, along with local community leaders, identify people who could benefit from POSER support through home visits, checkups at local health facilities, connections with local government, and community-based organizations. POSER staff register eligible people in the program and conduct a vulnerability assessment to gauge which needs are most urgent.
Once support begins, POSER staff ensure the continuity and effectiveness of care by regularly visiting patients and families at their home. Using a mobile health app, Medic Mobile, CHWs have already registered more than 76,000 individuals to track their ongoing care in more than 16,000 households since 2019—with more added on a regular basis.
One Stop Health Care

APZU’s Integrated Chronic Care Clinic (IC3), launched in 2015 as a collaboration with Malawi’s Ministry of Health, brings patients for asthma, hypertension, diabetes, mental illness, and other non-communicable diseases under one roof for treatment that is intertwined with HIV care across 14 health facilities in Neno District. This integration takes into consideration chronically ill patients’ needs for one-stop care and diminishes stigma associated with specific conditions. In a three-year study of the integrated care model, clinical measurements—such as blood pressure, asthma severity, blood sugar, or number of seizures per month, for patients with epilepsy—showed statistically significant improvement. One year after enrolling in IC3 care, more than half of hypertension patients had controlled blood pressure, and patients with epilepsy were reporting fewer seizures overall—with more than 40% regularly reporting no seizures since their previous visit.
Starting in 2019, trained mental health counselors began screening mothers for depression at routine antenatal visits as part of this comprehensive approach. So far, 91 people have participated in the group Problem Management Plus (PM+) intervention and preliminary data show that over 90% of patients’ depression improved from moderate and severe to minimal or no depression at all after the intervention. Data also indicate that over 90% of patients who benefited from the intervention remained stable with no depression six months after completing the group therapy program.
Sexual and Gender-Based Violence

In 2019, to address widespread sexual and gender-based violence (SGBV), APZU launched a program called No Woman or Girl Left Behind. In addition to supporting SGBV survivors, the program also aims to advance sexual and reproductive health and rights for adolescent girls and advocates for those rights nationwide.
APZU established a gender-based violence task forces in all health centers across Neno District, each bringing together health workers, social service providers, and police in one place. Previously, these services were sometimes located hours apart, making such support inconvenient and largely inaccessible. Now, patients are offered a menu of services at nearby sites, including testing for sexually transmitted infections, HIV post-exposure prophylaxis, pregnancy testing, social support, and psychological counseling.
From January 2020 to December 2021, Neno’s SGBV team worked on 228 such cases, including 26 victims under 10, and 48 cases involving victims under 14.
HIV/AIDS

When clinical and support staff began caring for people living with HIV/AIDS in 2007, the conventional wisdom among global health officials was that treatment was not an option in impoverished communities. “Focus on prevention” was a common refrain for decades. But this mindset would have left millions of people worldwide without care; it is a worldview PIH refused to accept.
Malawi has one of the world's highest rates of HIV. Specifically in Neno District, 1 in 10 residents live with the virus, and many used to struggle to access medications and the care necessary for long-term survival. For the past 15 years, APZU has worked with community health workers and Malawi’s Ministry of Health to provide comprehensive care in 14 health facilities, including more HIV tests and access to treatment.
As of late 2021 in Neno district, 94% of people living with HIV (ages 15-49) were enrolled in life-saving antiretroviral treatment; in 90% of these patients the virus was undetectable.

