World TB Day: A Q&A With Expert Carole Mitnick
Posted on Mar 22, 2013
In 2011, more than 8.5 million people became sick with tuberculosis and 1.4 million people died from it, according to the World Health Organization. That same year, according to WHO estimates, 630,000 people were sick with multidrug-resistant tuberculosis (MDR-TB), a hard-to-treat bacterium that’s becoming more prevalent and can take two years to cure. Fewer than 5 percent of MDR-TB patients receive appropriate treatment.
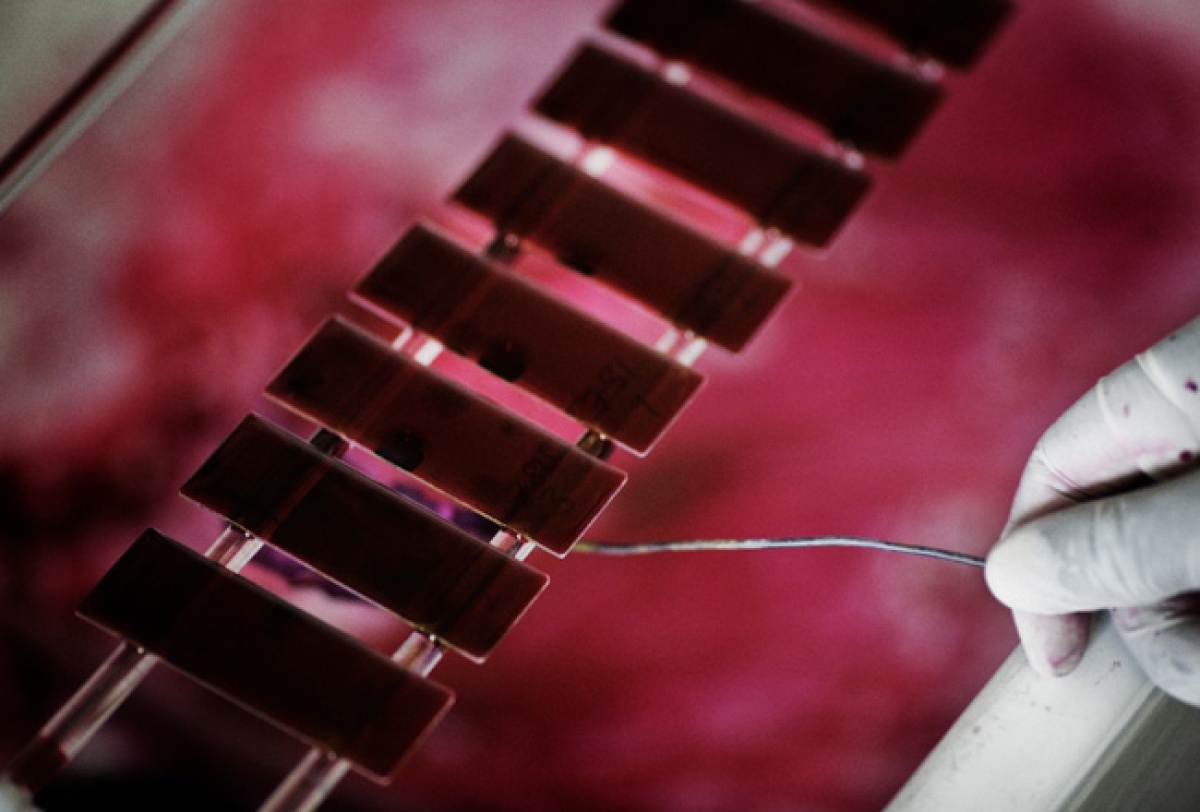
Despite the burden of MDR-TB, few drugs exist to treat it. On December 28, 2012, the U.S. Food and Drug Administration conditionally approved bedaquiline as part of a treatment regimen for adults with MDR-TB. It is the first drug to garner FDA approval for MDR-TB and the only tuberculosis drug to come to market since 1970.
As World TB Day approaches, Partners In Health spoke with Carole Mitnick, a TB researcher and assistant professor of global health and social medicine at Harvard Medical School, our longtime academic affiliate and partner. Mitnick discussed the factors behind the dearth of new drugs, the benefits of community-based TB treatment models, and the myriad challenges associated with pediatric TB patients.
Q: First, can you explain the difference between tuberculosis, multidrug-resistant tuberculosis, and extensively drug-resistant TB?
The distinction lies in the drugs that are useful to treat this bacterial disease. TB is usually treated with a four-drug, six-month regimen. Upwards of 85 percent of people with TB can be cured with this regimen.
Multidrug-resistant TB is caused by bacteria that are resistant to the two most important drugs in the standard regimen, isoniazid and rifampin. Patients with this form of disease usually have to be treated for 18-24 months, with regimens containing at least five drugs. A lower percentage of patients with this form of TB are typically cured—on average just over 60 percent. Many others die. This is because the drugs are more toxic, less effective, and the disease is often more advanced by the time patients receive proper treatment.
In extensively drug-resistant TB (XDR-TB), the bugs are resistant to the two most important drugs in the standard treatment and the two most important drugs in MDR-TB treatment. These patients often receive treatment for 18-24 months, again with regimens containing at least five drugs, many of which are very toxic and of questionable efficacy. Cure is assured in even fewer of these patients—usually less than 50 percent.
Q: Is the number of MDR-TB and XDR-TB cases around the world increasing? Are certain regions becoming more prone to MDR-TB and XDR-TB?
All signs point to a growing global burden of MDR- and XDR-TB. The burden is usually thought about in two ways: percent of all TB cases that are MDR and XDR or absolute number of MDR and XDR cases. Percentages are low in most of Africa and Asia. But the absolute number of TB cases is so high that MDR among small percentages translates into hundreds of thousands of cases of MDR-TB each year. Moreover, in Africa, the joint HIV epidemic leaves millions exceptionally susceptible to all forms of TB, and to repeated bouts of TB or MDR-TB. Aggressive treatment of both diseases, such as that provided at PIH/Lesotho, is essential to save individual lives and impact the epidemic.
In Eastern Europe and the former Soviet Union, absolute numbers of TB cases are low, but the percentages of TB cases that are resistant are extremely high and growing. PIH’s Tomsk, Russia, site is, however, one of the shining examples in the region. In the years since PIH intervened, the incidence of TB, the proportion of TB cases that are MDR, and the incidence of MDR have all declined! That’s largely from working with partners to develop a unique ambulatory model to serve prison and civilian populations in the region.

Carole Mitnick, a TB researcher and assistant professor of global health and social medicine at Harvard Medical School. Credit:Suzanne Camarata
Q: Why has drug development, particularly for drug-resistant strains, been slow? Is there a lack of funding, a lack of scientific know-how, or political roadblocks?
There are two primary contributors to this problem, which are linked. First, TB is a disease of the poor. The market for anti-TB drugs, largely governments in Africa and Asia, is not seen as a “paying market” with significant profit potential for the pharmaceutical industry, which is motivated by profits.
Second, advocacy for new anti-TB drugs was virtually non-existent until about 10 years ago. The prevailing attitude among those responsible for global TB policy has been that what we had—a six-month, four-drug regimen good for most patients—was the best we could hope for. The battle in TB control, its architects maintained, was simply about rigorous, widespread delivery of the existing tools: drugs that are more than 50 years old; a diagnostic that is now more than 125 years old; and a vaccine that is more than 100 years old. There was a mentality of scarcity among those most concerned about TB, which seemed to preclude demands for innovations in treatment, diagnosis, and prevention. Since drug and medical device research and development is a lengthy process, this drought of imagination has delayed harvest of new technologies for decades.
Q: How significant is the FDA’s conditional approval of bedaquiline?
This is exciting for three reasons. First, symbolically: The approval of the first new anti-TB drug in nearly 50 years is a huge breakthrough, demonstrating that at least one profit-driven company saw value in pursuing a TB indication. Second, it created a regulatory precedent for approval of MDR-TB drugs. Last, and most important, it means that there is an alternative to the current regimens that have high toxicity and inadequate efficacy. There is even the potential that this new drug, and others in the pipeline, could shorten treatment. This would be an important achievement for patients and TB programs currently struggling to complete two years of treatment.
Q: Have you see anything in the early studies of bedaquiline that raises red flags?
The primary issue that dampens my enthusiasm is safety. We know that bedaquiline has potential heart toxicity. And too few patients have been evaluated to really know how safe the drug is, across populations. It should be noted that in the small clinical trials, more patients who received bedaquiline died when compared with patients who received the placebo. This does not mean people shouldn’t get the drug; it merely reinforces that all people who receive this drug as part of an MDR-TB treatment regimen need to be assured the highest standard of care and vigilance while receiving it.
Q: The FDA approved bedaquiline for adults. What about pediatric patients? What treatment options are available for children who have drug-resistant TB?
This is an enormously important issue. Anti-TB drugs have almost never been tested explicitly in children or developed for delivery to children. To comply with current FDA requirements for approval of bedaquiline, Janssen Therapeutics [the manufacturer of bedaquiline] has developed a plan to study new drugs in children. Rarely, however, do these plans get implemented. So, clinicians around the world treat based on their best guess for whether and how much of existing drugs to use in children. Pills are cut and crushed, capsules are opened, and medications are stirred into formula, juice, or food.
These practices are extremely imprecise and time-consuming. A TB nurse who works in a public health center that collaborates closely with Socios En Salud, our PIH sister project in Peru, estimated that it takes her a full day to create a week’s worth of doses for a single pediatric MDR-TB patient she is treating. What’s worse is that since children are thought to be “epidemiologically insignificant,” meaning they don’t tend to transmit disease, we have no idea how many children in the world actually have MDR-TB and what treatments they’re receiving. A year-old project by PIH collaborators at Harvard Medical School, called the Sentinel Project for Pediatric Drug-Resistant Tuberculosis, aims to answer these and other critical questions.
Q: Do you see foresee challenges to making bedaquiline available in resource-poor environments?
There are challenges, yes, but they are by no means insurmountable. We’ll need to subvert a tension that has plagued TB control efforts—that is, between providing the best treatment possible to all those who need it and a perceived need to protect against emerging resistance. TB policy has typically favored caution against resistance, which has meant restricting access to the most effective treatments. In contrast, in HIV, since treatment became affordable, the balance has mostly been on the side of providing treatment to as many as possible.
PIH and other partners working within a framework of equity and innovation will need to assure, first and foremost, that effective treatment is delivered widely. Our framework will need to complement the dissemination emphasis with safeguards that assure the new drug is used in a way that minimizes the risk of development of resistance and maximizes patient safety. This is completely consistent with the model PIH and our Haitian sister organization Zanmi Lasante piloted in Haiti, and then brought to scale in Peru; Tomsk, Russia; and Lesotho.

A patient in Lesotho with multidrug-resistant tuberculosis receives care from PIH/Lesotho staff. Credit: Pep Bonet/Noor
Q: Aside from slow progress on drug and diagnostic development, what other obstacles persist in fighting TB?
Although approximately 500,000 new MDR-TB cases occur each year, a small fraction—less than 5 percent—are thought to receive appropriate treatment. Obstacles include weak healthcare systems without proper investments, collaborations with other sectors, or support to facilitate the distribution of drugs, diagnostics, and information. And we can’t ignore underpaid and overworked providers whose capacity to provide quality care is limited by failures to situate them properly to deliver the promise of health as a human right.
Q: And what’s the concern over hospital-based models for TB care?
Continued reliance on hospital-based models is guaranteed to stymie scale up of treatment because the need far outpaces hospital-bed capacity, by orders of magnitude. This gap manifests, in many countries, in MDR-TB treatment waitlists that are hundreds or thousands of patients long. The justification for hospital treatment is often to remove infectious MDR-TB and XDR-TB patients from the community. The deep flaws in this logic are that while awaiting treatment, both before and after diagnosis, these patients have been in their communities already infecting family and neighbors.
Furthermore, hospitals in high-burden TB settings rarely have effective infection control measures to prevent transmission to other vulnerable patients, family members, and staff. Lastly, effective treatment is the best prevention: Once appropriate treatment is initiated, the risk of transmission to others declines precipitously. This has been demonstrated most recently by PIH affiliate Edward Nardell, who presented such findings at the World TB Conference of the International Union Against TB and Lung Disease.
Q: What are some of the clear advantages to the community-based model?
Delivering MDR-TB care in the community—as PIH and partners do in Peru, Haiti, Lesotho, Russia, and Kazakhstan, among other sites—has many benefits, beyond the transmission ones described above. Among the most apparent benefits is that it’s less disruptive to patients and families. Community care also provides a platform for comprehensive services, including attention to the social and economic needs that almost always coincide with medical ones. Working closely with the community creates opportunities for education, which remove stigma around the disease and accelerate diagnosis of additional cases. The success of bedaquiline introduction, and global MDR-TB treatment scale up, depends on expansion of care from hospital to ambulatory models.

