StopCOVID: Prioritizing Health Equity to Overcome the Pandemic
The COVID-19 pandemic has exposed stunning gaps in the U.S. public health and health care systems and highlighted the negative effects of hundreds of years of structural inequities and systemic racism on our communities. The U.S. COVID-19 response has been marked by politicization of public health, skepticism of science, and a lack of a national plan. In addition, COVID-19 and the economic precarity it has unleashed exacerbate profound racial and economic inequities with fatal consequences. The United States has now entered a dramatic third wave of COVID-19, with more cases per day and hospital admission rates higher than ever before.
Partners In Health has been deeply involved in mitigating the impact of COVID-19 around the world and in the United States. In Massachusetts, we stood up and scaled a state-wide program that has supported Governor Charlie Baker’s vision of a comprehensive response to COVID. We have scaled contact tracing on the Navajo nation in support of President Nez. In North Carolina, Illinois and Ohio we are supporting Departments of Public Health, and in cities and counties--from Newark to Montgomery, Fulton County to Collier County we have helped to build robust testing and contact tracing programs that center on equity through resourcing the most vulnerable people to effectively quarantine and isolate when necessary.
As the Biden-Harris COVID-19 Task Force assembles to chart the COVID-19 response in 2021 and beyond, to overcome COVID-19, save lives, reopen schools and businesses, we must ensure an equity-centered response: from community mitigation to testing and tracing to safe quarantine, working and sharing lessons with nations around the world. Equally, American investment must be restored in the global response to COVID-19 and in preparing for pandemic threats. Partners In Health is encouraged by the priorities in the Biden-Harris plan and submits the following recommendations:
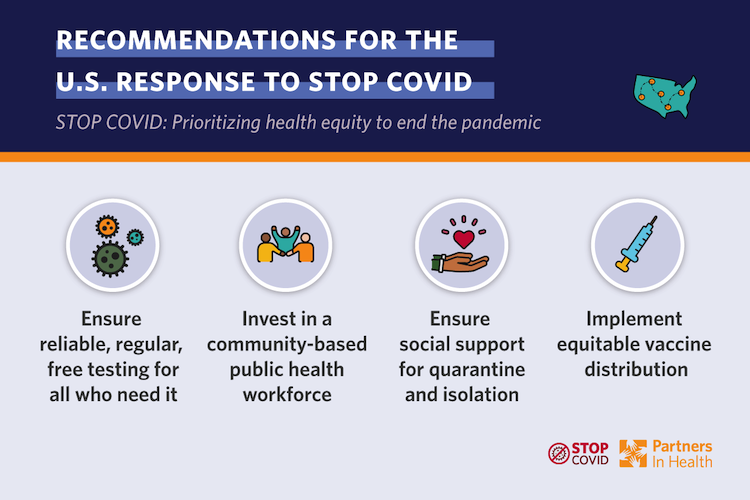
Recommendations for the U.S. Response to Stop COVID-19
1) Ensure everyone in America has access to regular, reliable, and free testing. The U.S. response to COVID-19 has lacked a coordinated, centralized effort, resulting in slow test uptake, inconsistent testing guidance, long turnaround times, and mixed results in billing. Testing is the critical first step in a full COVID-19 care cascade but must be followed by case investigation, contact tracing, and supported quarantine or isolation. Yet public health departments are ill-equipped to implement the range of interventions necessary.
To strengthen the testing and public health response, we recommend interventions that:
- Decrease testing turnaround time to under 24 hours by scaling up lab capacity for molecular and rapid tests, providing approval and guidance for rapid tests in both symptomatic and asymptomatic individuals, and incentivizing labs by structuring reimbursement based on turnaround time;
- Ensure access for everyone who needs a test by increasing testing capacity in communities of color, rural areas, and poor neighborhoods. Testing must be free or affordable to everyone, regardless of insurance status, and must not be limited by immigration status;
- Implement a National Purchasing and Dissemination Strategy to help states purchase and disseminate tests and medical supplies, without putting the full logistical and financial burden on states. Instead, there should be a national purchasing strategy for testing and medical supplies, and allocation of those resources should be based on data and state-specific needs.
2) Establish a well-paid, large public health workforce with a public health jobs corps and community health workers, hired from hard-hit communities. The Biden-Harris campaign plan included the creation of 285,000 jobs, however the growth of this crisis and deep systemic failures call for bolder proposals to dramatically increase the size of our health workforce. These roles should be recruited directly from communities most impacted by structural racism, which are facing higher rates of COVID-19, and are often culturally and linguistically diverse.
- More than 250 organizations and 143 Democrats in the House and Senate recently endorsed a Dear Colleague Letter calling for this workforce, among other key priorities, in response to the pandemic.
3) Ensure care is the center of the COVID-19 response by ensuring everyone is provided with the social and economic supports required to safely quarantine or isolate. Protect older Americans and those at highest risk through a highly integrated response. This response spans community spread prevention, testing, contact tracing, and supported quarantine and isolation. The economic downturn spurred by COVID-19 has caused nearly 12 million people to lose health insurance. Many others have suffered from inequities in the COVID-19 response due to underlying racial and geographic barriers to care. Ensuring that people have affordable health insurance coverage, transportation, and adequate access to care facilities such as well-funded federally qualified health centers, is pivotal to ending transmission.
We recommend the following interventions to help communities better respond to COVID-19:
- Accelerate equity-centered investments in contact tracing capacity, preferentially employing and engaging hardest-hit communities, in partnership with trusted community-based organizations. The Community COVID Care Act (and the updated HEROES Act) develops one possible approach and could work in coordination with the transition team’s proposed COVID-19 Racial and Ethnic Disparities Task Force.
- Invest in social support programs and care coordination to enable safe, supported isolation and quarantine, by providing financial assistance, childcare, food, housing, access to health care, and paid family leave to those affected by COVID-19. Nearly 20% of those infected with COVID-19 require additional resources to isolate at home. If left unsupported, these individuals risk perpetuating the epidemic as they buy groceries, care for family members, and work to sustain their lives. We must strengthen social support programs so all COVID-19 affected individuals and their contacts can meet the necessary isolation and quarantine requirements. This requires:
- Sustained funding for existing social programs, such as SNAP, unemployment benefits, federally qualified health centers, Medicaid, CHIP, rental assistance, and temporary economic assistance;
- Extended benefits for those affected by COVID-19. For example, North Carolina has set up support services for people who need assistance to isolate or quarantine, and these could be scaled with federal funds or guidance;
- Hiring and/or repurposing a workforce of patient navigators and cross-training contact tracers and case investigators to connect those in need to resources that are essential for effective quarantine and isolation;
- Reimagined COVID-19 care in carceral settings, including by releasing non-violent offenders. The Federal Correctional Facilities COVID-19 Response Act lays out a framework for further developing guidance for the Department of Corrections, based on public health recommendations.
4) Plan for the effective, equitable distribution of treatments and vaccines — because development isn’t enough if they aren’t effectively distributed. We urge the incoming administration to consider access and affordability at home and abroad. A comprehensive approach must include a distribution plan that addresses distrust of medical institutions in the U.S. That distrust, along with broad anti-vaccine sentiment and disinformation, require a large-scale investment in communication and community engagement, led in part by the same public health workforce discussed previously. Communities most impacted by historical harms must be engaged immediately to ensure uptake of vaccines and mitigate against exacerbating inequities. We recommend a vaccine distribution approach that encompasses planning and resource allocation, community mobilization, vaccine delivery, and individual and community follow up, with a focus on the most marginalized communities. The Biden-Harris administration must also combat monopoly barriers to production and sale, and coordinate the purchase and procurement of vaccine doses to enable rapid access and competition worldwide.
Recommendations for the global response to stop COVID-19 and prevent pandemic threats
COVID-19 should serve as a wake-up call: one of the best investments the U.S. can make for achieving a healthier, more secure, and peaceful world is strengthening health systems globally. Measures to predict, prevent, and mitigate pandemic threats outlined in the Biden-Harris plan including re-launching USAID’s PREDICT program, restoring the Directorate of Global Health Security and Biodefense and the U.S.'s relationship with the World Health Organization. All are critical. However, as the most explosive conditions for outbreaks are weak health systems and entrenched health disparities, improving health systems to deliver high quality care must be an integrated part of the pandemic preparedness and response strategy.
The following recommendations are key to responding to COVID-19 and preventing and responding to inevitable future threats globally:
1) Establish a commission to develop a new vision and framework for improving the efficacy of USG global health investments and reduce health inequities. Current U.S. global health funding modalities are outmoded. An new system should transition from disease-specific approaches – artifacts of the Millennium Development Goals – to an integrated health system strengthening approach as indicated by the Sustainable Development Goals for achieving universal health care and integrated health care delivery systems.
2) Increase investments in global health to at least $50 billion annually, in alignment with global funding commitments. Inadequate global health resources result in funding minimal interventions considered “sustainable” based on the limited health budgets of impoverished countries. This opens the door to and drives epidemics. While governments must raise maximal resources, for many low-income countries there is simply not enough tax capacity to fund universal health coverage and functioning health systems. A U.S. commitment of $50 billion annually represents approximately a four-fold increase in global health spending. It would increase the U.S. official development assistance to 0.7% of Gross National Income, a target agreed to by the world’s wealthy nations and the United Nations in 2005. An investment at this size could influence other nations, who have not already done so, to make this same commitment.
3) Improve international cooperation for COVID-19 response. Effective international cooperation requires the U.S. participating and collaborating in solidarity with other countries through the following measures:
- Ensuring a fair and equitable global distribution plan of COVID-19 vaccines and treatments;
- Using U.S. voting power and influence at international financial institutions to approve a large issuance of Special Drawing Rights and provide debt relief that fairly restructures and resolves heavy debt burdens, which cripple countries’ abilities to respond to health emergencies and invest in health systems; and
- Restoring U.S. membership in and funding to the World Health Organization and the Pan American Health Organization including payment of all contributions in arrears, in recognition of the significant resources, technical cooperation and solidarity needed to respond to COVID-19.
More than 250 organizations and 143 Democrats in the House and Senate recently endorsed a Dear Colleague Letter calling for reforms to our global health system, among other key priorities, in response to the COVID-19 pandemic.
Partners In Health stands poised and ready to help advance an equity-focused policy agenda with the incoming administration and the 117th Congress.
Please reach out to Justin Mendoza, U.S. Advocacy Manager - jmendoza@pih.org - with any immediate questions or if we can be of assistance in developing specific technical proposals on any of the above stated priorities.
