Op-Ed: Racial Justice Requires an Equitable COVID-19 Response
Death toll reveals deep racial injustice in America’s health care, housing, employment systems
Posted on Apr 29, 2021

The following op-ed was written by Dr. Joia Mukherjee, Partners In Health's chief medical officer, who is helping lead the organization's efforts to stop the spread of COVID-19 in the United States, through the U.S. Public Health Accompaniment Unit, and across 11 PIH-supported countries around the world. This op-ed was inspired by research Mukherjee conducted and published in the Harvard Health Policy Review.
Racism is the chronic and foundational crisis on which our country is built. The death toll of COVID-19 further reveals the deep racial injustice in America’s health care, housing, and employment systems.
America’s abysmal response to the pandemic was not a failure per se, but a political choice: wealth over bodies, specifically white wealth over Black, indigenous, and Latinx bodies. In the first year of the pandemic, among the 550,000 deaths, Black, indigenous, and Latinx people have suffered two to three times the mortality rate of white Americans. Similarly, the staggering economic pain and hardship of the fiscal freefall has had an outsized burden among these same communities.
The root cause of the disparities is clear: racism is embedded in our justice system, economic system, education system, and health system.
That is why a universal response to COVID-19—the same plan for everyone—will continue to exacerbate inequity. Rather, racial justice in our response to COVID-19 demands that we acknowledge that current inequalities are based on a racist system. And that we work together with people who suffer racial oppression to materially resource our response.
At Partners In Health, a global health and social justice organization, we have more than 30 years of experience working with affected communities to develop and deliver targeted approaches to achieve health equity and the plagues that disproportionately affect victims of historical and present day injustice. Whether fighting tuberculosis in Peru, HIV in Haiti, or Ebola in West Africa, resources for critical necessities such as food, transport, and housing are as necessary as are policies such as decarceration and community-based outreach.
Risk mitigation in the pandemic requires social distancing—this is most effective when people can stay at home. Yet so-called essential workers, 50% of whom are people of color, were required to be at work, often in the over-crowded conditions such as meat packing plants and farm worker camps. These jobs in food, agriculture, and transportation are often compensated at minimum wage or less and are without sick leave or benefits. In many European countries, people were compensated to stay at home. Yet in the U.S., only one payment was afforded to people in the first year of the pandemic.
The pernicious effects of racism on housing, food security, and political marginalization result in a much higher rate of pre-existing medical conditions in communities of color. And racist policies since the founding of the nation result in poor access to health care in Black, Indigenous, and Latinx communities. The impact of the social forces and the lack of health care access results in lower testing rates, higher case positivity, and delayed presentation with COVID-19. And now, with the vaccine rollout underway, we see yet again the stark inequities. An analysis in early March found the vaccination rate for Black Americans is half that of white people, and the gap for Latinx people is even larger.
Then there was Donald Trump. The former president’s racist policies and the blame he leveled at China -- describing the virus as the “Kung Flu” -- resulted in attacks against Asian Americans, such as the horrific Atlanta spa shootings in March.
Amidst a longstanding void of federal leadership in the Trump Administration, some local communities laid the path for the way forward in targeting assistance to the most vulnerable.
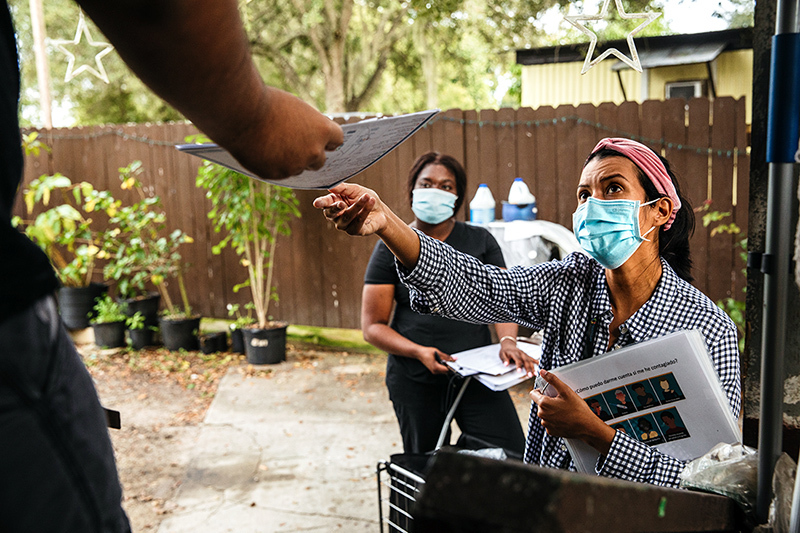
In rural Immokalee, Fla., the Coalition of Immokalee Workers, an organization of migrant and essential workers disproportionately hit by COVID-19, partnered with Healthcare Network, the local Federally Qualified Health Center, to establish a new community health workforce to go door-to-door supporting those most at risk, to expand access to testing, and to register and help transport eligible individuals to vaccination programs.
In counties across North Carolina, community health workers and organizations providing social supports, partnering with the state, have reached 35,000 households with bags of groceries, prepared meals, masks, hand sanitizer, thermometers, and relief checks. Preliminary findings from an ongoing statewide analysis suggest that N.C. counties with these social supports have lower COVID-19 case positivity rates.
Lifesaving vaccines are now available, but distribution has been chaotic at best, deeply unfair at worst. Many communities need help developing equitable vaccine distribution plans and community engagement strategies to establish public trust, especially in historically marginalized communities. Cook County, Ill., is working to identify “vaccine deserts” in impoverished neighborhoods and then mobilize resources to remove this barrier to care. In Newark, N.J., the city is deploying pop-up vaccination sites to homeless shelters and senior housing buildings, making vaccination accessible and bringing doses directly to communities so that those at higher risk can easily roll up their sleeves to receive protection.
At PIH, via our U.S. Public Health Accompaniment Unit, we’ve been pleased to support urgent requests for targeting assistance to the most vulnerable in communities across the country. Without community-level interventions to resource those impacted by the structural racism of the United States, current systems will exacerbate inequities and further shift the burden of COVID-19 to people of color.
Efforts that restore equity and focus on justice must continue.
To improve health, bolster our public health systems, and truly be prepared for future outbreaks, we must undo racist policies and focus on repairing the harm that has already been done.
About the Author
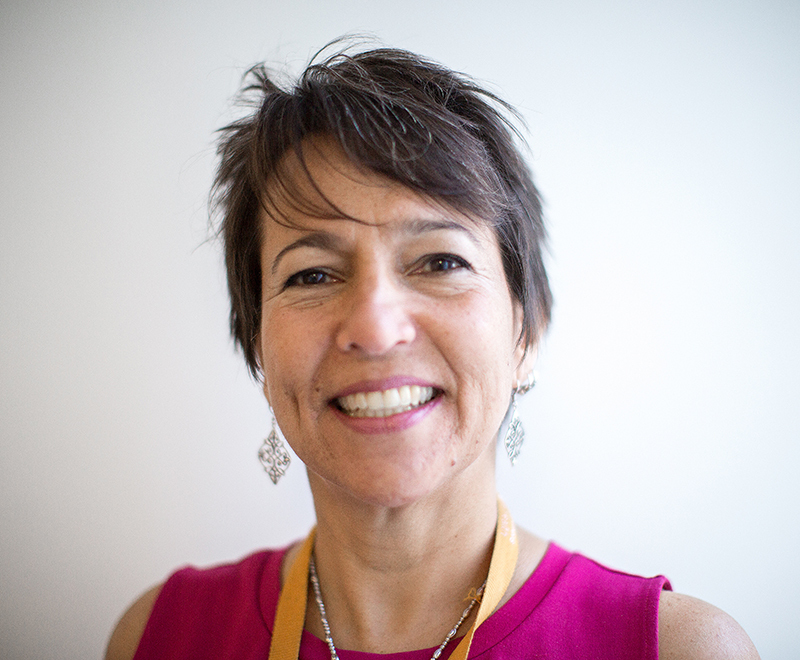
Dr. Joia Mukherjee is PIH's chief medical officer and an associate professor of medicine at Harvard Medical School. She is also the author of An Introduction to Global Health Delivery.

