Vaccine Eligibility Does Not Guarantee Access
Why and How to Prioritize Those Most at Risk in COVID-19 Vaccine Rollout
Posted on Apr 29, 2021

Every adult in the United States is now eligible for COVID-19 vaccines -- a critical milestone. As the nation races against a fourth wave of the virus and increasing spread of variants, vaccinating the entire population is as urgent as ever.
But eligibility alone does not guarantee access.
Already, among equally eligible people within states, the wealthy are getting vaccinated far faster than others. Eligibility won’t improve health disparities, and it could perpetuate long-standing inequities rooted in this country’s structural racism
In a new white paper on vaccine equity, Partners In Health’s U.S. Public Health Aaccompaniment Unit (USPHAU) leaders make a powerful case that both epidemiologic evidence and justice demand the prioritization of certain groups in the ongoing vaccination process, specifically older adults, communities of color, and essential workers.
An Inequitable Rollout
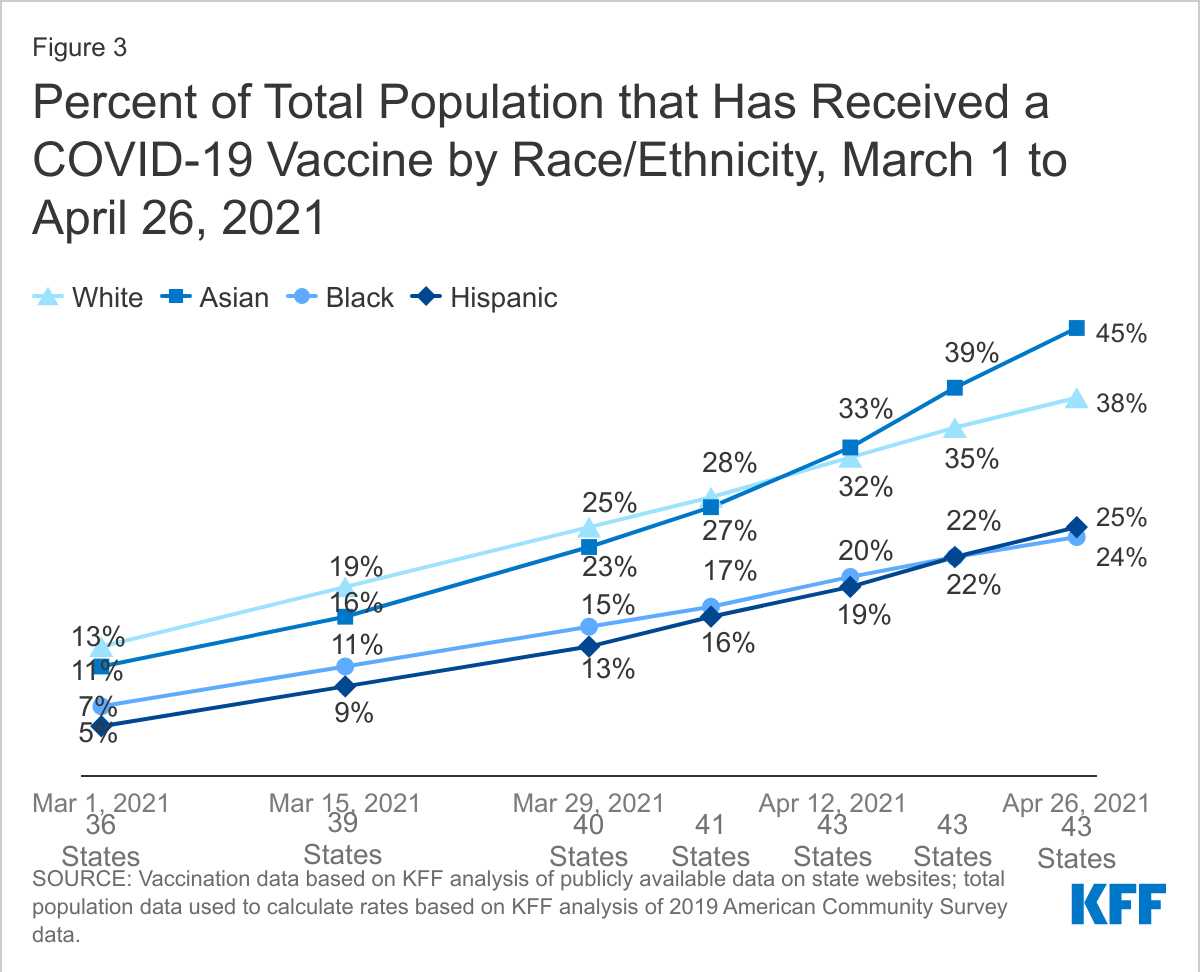
According to a Kaiser Family Foundation analysis of vaccination uptake in 43 states, “the percent of White people who have received at least one COVID-19 vaccine dose (38%) was 1.6 times higher than the rate for Black people (24%), and 1.5 times higher than the rate for Hispanic people (25%) as of April 26, 2021.” Following the same trends seen throughout the pandemic – from access to testing sites to acquisition of personal protective equipment -- vaccination rates remain low in many of the hardest-hit communities. Without intervention, vaccination rates in these communities will continue to lag behind and worsen inequities.
The intersection of marginalized identities, including race, age and employment, compounds poor health outcomes. The risk of death from COVID-19 increases sharply with age, with greater than 80% of reported deaths in the U.S. among those 65 and over. Risk-based vaccination also dictates prioritizing Black, Indigenous, and Latinx communities, who have experienced two- to three-fold higher hospitalization and death rates from COVID-19 than the white community. Though the majority of U.S. COVID-19 deaths have been in the oldest age groups, the death rate among Black an Hispanic patients aged 65 and older has been a significantly higher share of those populations than compared to white patients, the paper notes.
Similar disparities in risk are evident among frontline essential workers, half of whom are from communities of color, with over-representation among jobs in major industries like energy, agriculture, and childcare that form the backbone of our society. Black workers in particular are more likely to have jobs with the highest risk of exposure to COVID-19. Essential workers are at heightened risk of both contracting and transmitting COVID-19 based on the nature of their work, making them a clear priority for vaccination.
A Social Justice Imperative
Racial and social justice reinforce the epidemiological evidence: historically marginalized groups have disproportionately suffered from COVID-19 and therefore deserve priority protection, the paper authors write. Whether discussing cancer, diabetes, or maternal mortality, the burden of disease born by communities of color is disproportionately greater in the U.S. Indeed, in the first half of 2020, non-Hispanic Black people had a six-year lower life expectancy than white populations in the U.S. Systemic injustices embedded in many U.S. institutions, which were initially built on slavery and codified by legislation, continue today, including in public health.
Generations of structural inequity and racism have culminated in limited access to health care in certain communities, the paper authors write. Already limited access is further compounded by logistical barriers. Take access to COVID-19 care as one example. Vaccine sites often operate with limited hours and are in difficult-to-reach locations with limited connection to public transportation. These barriers disproportionately affect essential workers who must balance job demands against opportunities to be vaccinated. Additionally, there are many barriers to vaccine access among older, non-English speaking, and disabled populations: internet access, advanced technology, and mobility are often requirements for scheduling and getting to appointments at most vaccine sites.
Population immunity is only achievable if every community has access to vaccines.
According to the white paper authors, the nation’s leaders have to ensure 70-90% of the population is vaccinated. To do this, they must eliminate structurally racist barriers and invest in community partnerships to achieve vaccine equity and to reduce transmission and disease burden throughout the country, especially in systematically marginalized communities.
From Theory to Practice, Making Vaccine Equity Work
Equitable vaccination is possible. PIH’s USPHAU, which provides technical support, assistance, and resources to tackle the COVID-19 pandemic, is collaborating with partners in cities, states, and communities across the nation where vaccination activities are in process. The shared goal is to address supply and demand challenges in equitable vaccination, while beginning the process of correcting historical health injustices. Many of these approaches are drawn from PIH’s global experience with community health, vaccination campaigns, and emergency response over the last three decades, from addressing the cholera outbreak in Haiti to the Ebola epidemic in West Africa.
Listening to Communities
Access to accurate and transparent information about the development, safety, and efficacy of the vaccine—as well as how to access it—is a critical element when attempting to build trust between community members and the public health system. Ultimately, all messaging and communication strategies must be tailored to specific community needs, questions, and concerns, and they should be developed in partnership with community members.
In Montgomery, Ala., USPHAU is working with the mayor’s office, the department of health, a social impact creative firm, and community leaders to develop a public engagement campaign, Level Up, that is specific to local needs. Key community members were interviewed to gain their perspectives on COVID-19 and vaccines. Their answers then informed surveys, social media, and other local messaging wrapped into the campaign, which launched as the state’s vaccine eligibility expanded. In addition, USPHAU helped launch a free rides program that offers transportation for community members, and a cadre of community vaccine ambassadors who provide vaccine education and appointment scheduling to navigate challenging sign-up systems.
Mind the Gap
Spatial mapping within communities and regions offers another way to identify gaps in access. This visual approach can spark discussion and drive collaborative planning for improving community access.
In Ohio, for example, USPHAU is helping coordinate across community, government, and academic partners to comprehensively document and visualize the resources and vaccination needs of communities most vulnerable to COVID-19. Because of this work, the team has identified where gaps in coverage exist and public transportation is insufficient, as well as proposed areas where mobile vaccination units are necessary to meet local vaccination goals.
In New Bedford, Mass., USPHAU is supporting vaccine site operations that focus on specific vulnerable communities, using low-tech tools and local knowledge to register and vaccinate individuals who lack access to technology and English language proficiency.
Building Long-Term, Equitable Health Systems
Ultimately, vaccination is just one part of a robust and effective COVID-19 response, and even the most optimistic predictions have domestic and global population-level immunity months and years off, respectively. Vaccination and booster campaigns will continue long after. While leaders continue to drive vaccine resources where they are most needed, they must also double down on other aspects of response, recovery, and reimagining public health.
On the Navajo Nation, where vaccination coverage has outpaced states, USPHAU is supporting contact tracers who incorporate questions on vaccination status into regular calls and training staff to solicit feedback, answer questions, and make referrals for COVID-19 vaccination.
In Pima County, Ariz., USPHAU is also incorporating vaccine messaging into contact tracing and case investigation calls to bolster community response to the vaccine. The team has helped the health department craft strategies, in collaboration with local community organizations, to reach vulnerable sub-groups of the population – including individuals experiencing homelessness, American Indian and Alaskan Natives, refugees, and those who are homebound.
Cecelia Rose English, the USPHAU senior team leader in Arizona, said that alongside local partners, her unit’s plan is to “ensure [a] vaccine is available to everyone in Pima County by May 2021.”
Breaking Down Barriers
In Immokalee, Fla., USPHAU and partners work at testing and vaccination sites to connect those in need to social supports, including food vouchers and unconditional cash transfers, to help them through isolation and quarantine and to alleviate the disproportionate impact of the pandemic on the community.
And in North Carolina, USPHAU is working with state partners to focus on the needs and barriers of vulnerable populations and ensure social and health services screening by community health workers becomes a standard practice during vaccine registration so that community members have what they need to stay safe and healthy.
Devin Worster, senior project lead in North Carolina, said the state is taking vaccine equity a step further. Officials are working with partners to encourage community health workers and community-based organizations “to provide vaccine education, schedule individuals for vaccine appointments, and host community vaccination events to best target marginalized populations in the communities where they live, at locations they will trust, and at the hours that are most convenient to them.”
Vision for the Future
In order to stop COVID-19 and achieve a new normal — opening businesses, schools, and communities — no one must be left behind, the authors argue. Population immunity can only be achieved with successful vaccination programs in every community, at the global, national, and local levels. Critically, these strategies cannot be one-time initiatives; they must be part of a durable effort to empower communities, as the most experienced and best positioned to advocate for structural, logistical, and educational resources that will not only increase vaccination coverage but also improve long-term health.

